1- What’s infertility?
Conception requires the fusion of a mature oocyte with a spermatozoid that leads to the formation of an embryo. Each month, an oocyte is ovulated from the ovaries and is released in the fallopian tube where it meets and gets fertilized by a spermatozoid. The resulting zygote will undergo its early embryonic development while migrating through the fallopian tube and it reaches at day 5 the uterus where it implants. So, to be able to conceive many steps starting from oocyte production and ovulation until embryo implantation have to be done successfully and pregnancy is not very easy to achieve. Hence, the fecundity rate for a couple having regular unprotected sexual intercourse varies between 20 and 25% each month. Infertility is a failure to achieve pregnancy after 1 year of effort.
2- What are the causes of infertility?
The factors contributing to infertility vary widely. Worldwide studies show that 35 % of infertility cases are explained by physiological causes in men and 40% by physiological causes in women. In approximately 15% of the cases both male and female factors are detected and in 10% no cause is found.
A preliminary study performed in Azoury IVF Clinic showed that in Lebanon, male contribution to infertility is higher. This can be due to the long years of war we went through and to the toxicity that is surrounding us.
|
|
|
3- What does infertility treatment involve?
Male infertility is generally diagnosed after a simple sperm testing and a hormonal blood test. If a problem is found, vitamins and/or hormones can be given but in most of the cases treatment generally requires Assisted Reproductive Technology (IUI, IVF or ICSI).
For woman of reproductive age, causes of infertility are very diversified. They can be ovarian, tubal, uterine cervical or peritoneal. Each cause of infertility requires a very specific treatment. Thus, a great understanding of the cause of infertility is required to be able to offer the patient the most personalized and adapted treatment to her case. Infertility treatment can vary from a simple lifestyle change and weight loss, to hormonal treatments, surgery or Assisted Reproductive Technology (IUI, IVF or ICSI).
|
|
|
|
|
|
4. Why do I have to take so many injections before an IVF attempt?
Each cycle, a woman generally ovulates only one egg. This egg can be of good or bad quality; it can get fertilized by the sperm or not; the embryo obtained can undergo normal early development or not; it can implant or not. Hence, when we undergo a burdensome IVF cycle, we stimulate the ovaries using hormonal injections in order to obtain a bigger number of oocytes and have better chances in obtaining a good embryo that will lead to a pregnancy.
 |
5. Do I lose follicles from my reserve if I undergo ovarian stimulation?
Definitely not! And this is a general misconception!
Each day a different group of follicles starts growing in a woman’s ovaries. The recruitment of these follicles and their first phase of growth are independent from hormones. When these follicles reach a certain size, their growth becomes dependent of hormones. The biggest and strongest of these follicles starts “taking all the hormones” produced by the woman’s body and continues to grow alone while the other follicles do not have “enough hormones” and die. The injection of hormones used during ovarian stimulation saves these follicles from dying but does not lead to recruiting more oocytes from the ovaries.
6. Why is there nearly always a difference between the number of follicles seen by ultrasound and the number of oocytes retrieved during oocyte pick-up for IVF?
Using ultrasound, the doctor can see the follicles and follow up on their growth. The follicles are not the oocytes, they are the “bag” that contains the oocytes and helps it become competent. It is impossible to see the oocytes by ultrasound. Some follicles are empty and that’s why there is very often a difference between the number of follicles seen by ultrasound and the number of oocytes retrieved during oocyte pick-up for IVF.
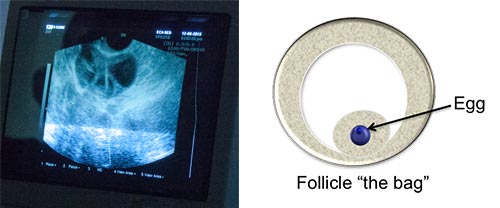 |
7. Does ovarian stimulation cause cancer?
Thousands of clinical trials have been trying to answer to this question and no clear-cut answer has been reached so far. However, it is admitted by many specialists that hormones that are injected during ovarian stimulation are not toxic and are unlikely to cause cancer. On the other hand it is strongly believed that hormones promote cancer in people that are suffering from it without knowing.
8. Why don’t good embryos always implant?
First, there is a big clarification that has to be made on the definition of a “good, or type A embryo”. In the past we used to judge embryos only based on their morphology. Now with the use of the Embryoscope we know that some embryos look good but are not good at all and do not implant.
Second, even “real” type A good embryos do not always implant even if we don’t have any problem at all. In fact, the embryo is transferred to the cavity of the uterus, the closest possible to the endometrium. However it has to implant IN the endometrium (which is rich in blood vessels) in order to receive nutriments from the mother’s blood and grow. The fact that the endometrium is rich in blood vessels makes it impossible to force the embryo inside it because there is a big risk of inducing damage to blood vessels that could lead to a loss of blood and a consequent loss of the embryo. Hence, all we can do while transferring an embryo after IVF is bringing it the closest possible to where it should be and hoping it will go the right way and implant.
9. What are the most common causes of implantation failure?
There are many known causes of implantation failure and most probably many causes that remain unknown. These are the most common ones:
- Bad quality embryos: these embryos are incapable of implanting and if they implant will most probably be rejected later on by the endometrium.
- Bad quality endometrium: this can be assessed by the doctor using ultrasound and can generally be avoided by an adapted stimulation protocol and an adapted hormonal treatment after transfer.
- Luck: As we clarified in the FAQ number 8, when the doctor is performing the embryo transfer he cannot put it where it should be but only close to where it should be and there is always a risk that the embryo goes the wrong way and fails to implant.
10. What does it mean when we have a positive pregnancy test that directly drops afterwards?
It means that the embryo has implanted and then has been rejected. The causes for this rejection are not all known but here is some of them:
- Bad quality embryos: Some of these embryos implant and then get rejected by the endometrium.
- A bad blood circulation and coagulation state that does not allow the embryo to grow appropriately: this can be solved by the administration of anticoagulants. However, it is not recommended to always take these anticoagulants and their intake should be closely followed by the physician.
- A strong local immunity: the embryo is a stranger to the mother’s body and a high immunity in the endometrium could lead to the rejection of the embryo. In Azoury IVF Clinic, we assess the immune state of the endometrium in collaboration with MatriceLab Innove in Paris and if an immune problem is found, the appropriate treatment is given.
|
|
|
11. What is Laser-Assisted Zona Pellucida Hatching and when is it recommended?
The Zona Pellucida is the envelope that protects the embryo. As the embryo grows, the Zona Pellucida becomes more and more thin so the embryo can “get out of it” and implant. Sometimes, the Zona Pellucida is very thick and does not allow the embryo to get out of it. In this case, it is recommended to perform a Laser-Assisted Zona Pellucida Hatching, that renders the zona thinner before transferring the embryo. However, it is not recommended to use this technique on all embryos especially the ones that are presenting a thin zona because internal cells of the embryo can be damaged by the laser shots. We, at Azoury IVF Clinic, perform assisted Hatching when it is necessary in a routine way, without asking the patient and without charging extra money for it.
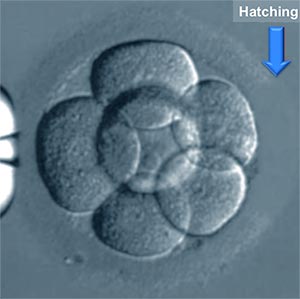 |
12. Why does IVF success rates decrease with advanced maternal age?
Advanced maternal age affects both the number and the quality of the oocytes leading to an automatic decrease in the numbers and the quality of the embryos obtained.
It is established that a woman is born with a “stock” of oocytes that was produced when she was a fetus in her mother’s womb. When she reaches a certain age the stock starts to reach its end this is why the quantity is reduced. The quality is reduced because some components that are present inside the oocytes become “expired” or get degraded and are not effective anymore. When oocyte quality is reduced there is no way back. However, a healthy lifestyle, and some vitamins and co-enzymes may protect the oocytes from getting worse to certain limits.
|
|
|
|
|
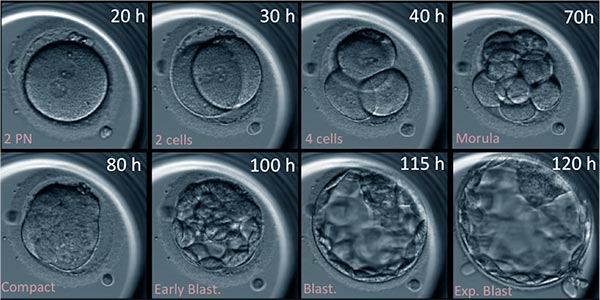
13. Do you transfer embryos on day 3 or day 5?
Each IVF laboratory follows its own embryo transfer strategy here is ours:
We are convinced that day 5 embryos that have reached the blastocyst stage have better implantation potential than day 3 embryos. Depending on the case and the number of obtained embryos, we decide if the transfer will take place on day 3 or day 5:
- If the patient has a lot of embryos on day 3 we schedule the transfer for day 5 for better embryo selection.
- If the patient has only 1 or 2 embryos on day 3, we do the transfer on day 3 as we believe that the conditions in the mother’s womb are better than any incubator and if there is no selection of embryos to be made it is better to transfer the embryos.
|
|
14. Is oocyte pick-up procedure painful ?
Oocyte pick is performed under local anesthesia and is not painful
15. Is embryo transfer procedure painful ?
The embryo transfer procedure is not painful
16. What do you offer for repetitive implantation failure after IVF treatment?
Repetitive implantation failure can be due to bad embryos and/or a “bad” endometrium.
If the ultrasound does not show any uterine or endometrial abnormality, we first suggest the use of the Embryoscope in order to have a real assessment of embryo quality that is not only based on their morphology but that takes into consideration the kinetics of their divisions. If the embryos appear to be dividing well on the Embryoscope we suggest an assessment of the immune state of the endometrium in collaboration with MatriceLab Innove in Paris. In fact, the embryo is a “stranger” to the woman’s body and a dis-equilibrated immune state can lead to its rejection.
 |
|
|
|
17. How is IVF Preformed ?
|
|
|
18. What is PCOS (Polycystic ovary Syndrome) and how should it be treated?
19. What is endometriosis and how should it be treated?
20. What is varicocele and should it always be treated?
21. What are the most common causes of Early pregnancy loss?
-Embryo chromosomal abnormalities
-Blood coagulation problems
-Elevated uterine immunity
-High Sperm DNA Fragmentation Index
22. What is the Endometrial Receptivity test? (ERA)
The endometrium is not always ready to receive the embryos and can only receive them in a specific timing called Window of Implantation. This Timing varies from a woman to another leading sometimes to repetitive implantation failure.
Undergoing an ERA test requires doing a whole mock cycle, the endometrium is prepared starting day 2 as if embryo transfer will take place and at the time of embryo transfer, instead of transferring embryos, a biopsy is taken from the endometrium and sent for receptivity testing.
23- What are Epigenetics and how do they affect the embryo in an egg donation cycle?
Epigenetics are the factors that affect the expression of genes without changing their code. In an egg donation cycle, the maternal genes of the baby come exclusively from the donor. However, the regulation of these genes and how they are expressed is under the control of the environment of the mother that is carrying the baby.
24- What is PRP and does it help?
PRP is used in different medical fields nowadays and has proven to be efficient in many of them. It stands for Platelet Rich Plasma. It is extracted from the person’s blood and activated in vitro then re-injected in the region of interest. Platelets secrete many factors that enhance the activity of the cells of this region and motivate them to work better. In the reproductive medicine field, PRP injection in the endometrium is proposed to improve its thickness which might increase embryo implantation while PRP injection in the ovaries is proposed to yield to better ovarian response during ovarian hyper-stimulation. Few studies have been published in these regards and efficiency is not proven yet. However, due to its safety and accessibility, PRP can be used as a last resort when no other medical treatment has succeeded.